How is the primary prevention of sexual violence linked to substance abuse, and how can we connect both of these public health issues?
As the Centers for Disease Control and Prevention (CDC) continues work around addressing opioid overdose, sexual violence preventionists and advocates continue to raise awareness about the link between sexual violence and addiction. While states are attempting to reduce supply through legislation, the demand created by the over-prescribing of opioid painkillers isn’t going away.
In a previous post, we highlighted the importance of involving community rape crisis centers in the response to overdoses due to opioid use, and talked about the limited amount of research and news coverage that is available connecting the opioid epidemic and sexual violence.
At NSVRC, our focus is on the primary prevention of sexual violence. Here is how we describe primary prevention:
“In the sexual violence field, we use the term “primary prevention,” which means stopping sexual violence before it even has a chance to happen. Primary prevention challenges out-of-date and victim-blaming attitudes that place the onus on potential victims to protect themselves and frames sexual violence as a public health issue.
Primary prevention requires that we make the connection between all forms of oppression (including racism, sexism, homophobia, ableism, adultism, ageism, and others) and how these create a culture in which inequality thrives and violence is seen as normal. Effective prevention efforts utilize prevention theories to change communities, shift social norms, end oppression, and promote norms of equity, consent, and safety for all.”
So how is the primary prevention of sexual violence linked to substance abuse? How do we connect both of these public health issues (sexual violence and the opioid epidemic)?
Pictures speak louder than words.
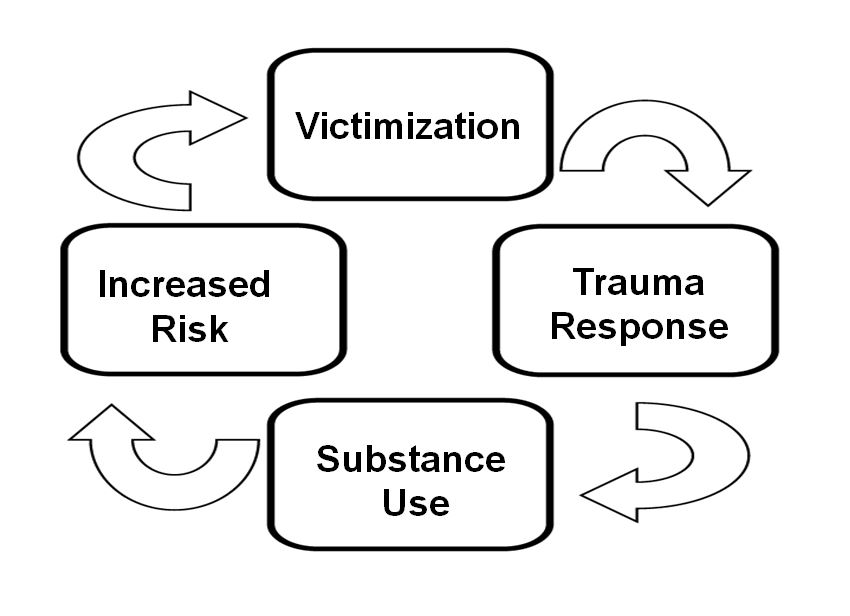
The image above represents the cycle many survivors of sexual violence with substance abuse issues find themselves in:
- A person experiences sexual violence
- Experiencing sexual violence can lead to ongoing traumatic responses for survivors.
- Survivors may use substances to self-medicate as a coping mechanism to suppress the impact of trauma.
- Substance use increases a person’s risk of experiencing sexual violence.
- This can lead to additional trauma, which can lead to increased substance abuse, and the cycle continues.
A person can enter this cycle at multiple points, when experiencing sexual abuse or when abusing substances. Regardless of how they enter the cycle, multiple victimizations may occur. Experiencing multiple assaults can make it harder to stop self-medicating through the use of drugs. If someone stops abusing substances, their trauma and thus the need to self-medicate is likely to resurface.
Preventing sexual violence or substance abuse from occurring in a person’s life is likely to prevent the other. Also, considering both substance abuse and sexual violence share similar risk and protective factors, there is great value in addressing substance use prevention when working to prevent sexual violence. Conversely, sexual violence should also remain part of the dialogue around the opioid epidemic.
It is common for those of us in various helping fields to focus narrowly on our “issue.” We list legitimate reasons for this: time, money, capacity, and so on. But the people we serve do not live in a silo. Many live with addiction; trauma related to sexual violence; and struggles related to poverty, racism, limited housing options, lack of childcare, few job opportunities, and many other forms of trauma. If the opioid epidemic impacts your work, consider reaching out to those doing sexual violence prevention, and vice versa. Those who are caught in the addiction and violence cycles need us to think more broadly about what our “issues” really are, so that prevention and healing can truly be possible.
This blog will be part of an ongoing series on the opioid epidemic. In this series, we will talk about the epidemic and sexual violence prevention, and offer guidance and tools for sexual violence advocates in addressing these issues.